Why Care Execution Matters More Than Care Management Alone
Why Care Execution Matters More Than Care Management Alone
Why Care Execution Matters More Than Care Management Alone
Why Care Execution Matters More Than Care Management Alone
Posted on :
Feb 2, 2026
Feb 2, 2026
Feb 2, 2026
Share on:
Share this Article :
Care management has become a standard part of modern healthcare. Most practices today have care coordinators, nurses, risk stratification tools, and documented care plans. Yet outcomes often remain unchanged. Hospitalizations continue, gaps in care persist, and staff feel stretched despite growing care management programs.
The difference is not effort or intent. It is execution.
Care management defines what should happen. Care execution ensures it actually happens, at the right time, for the right patient, by the right person.
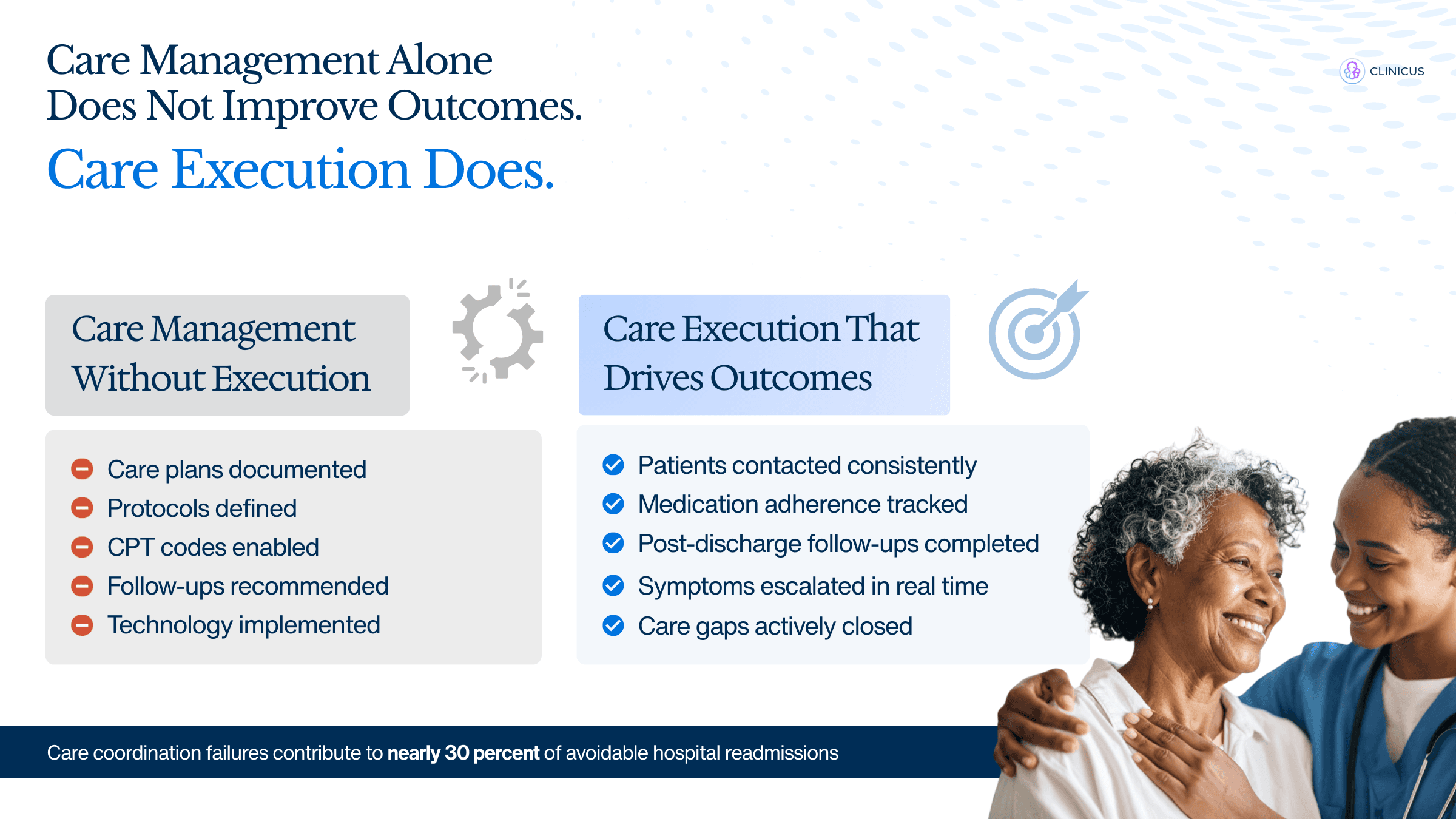
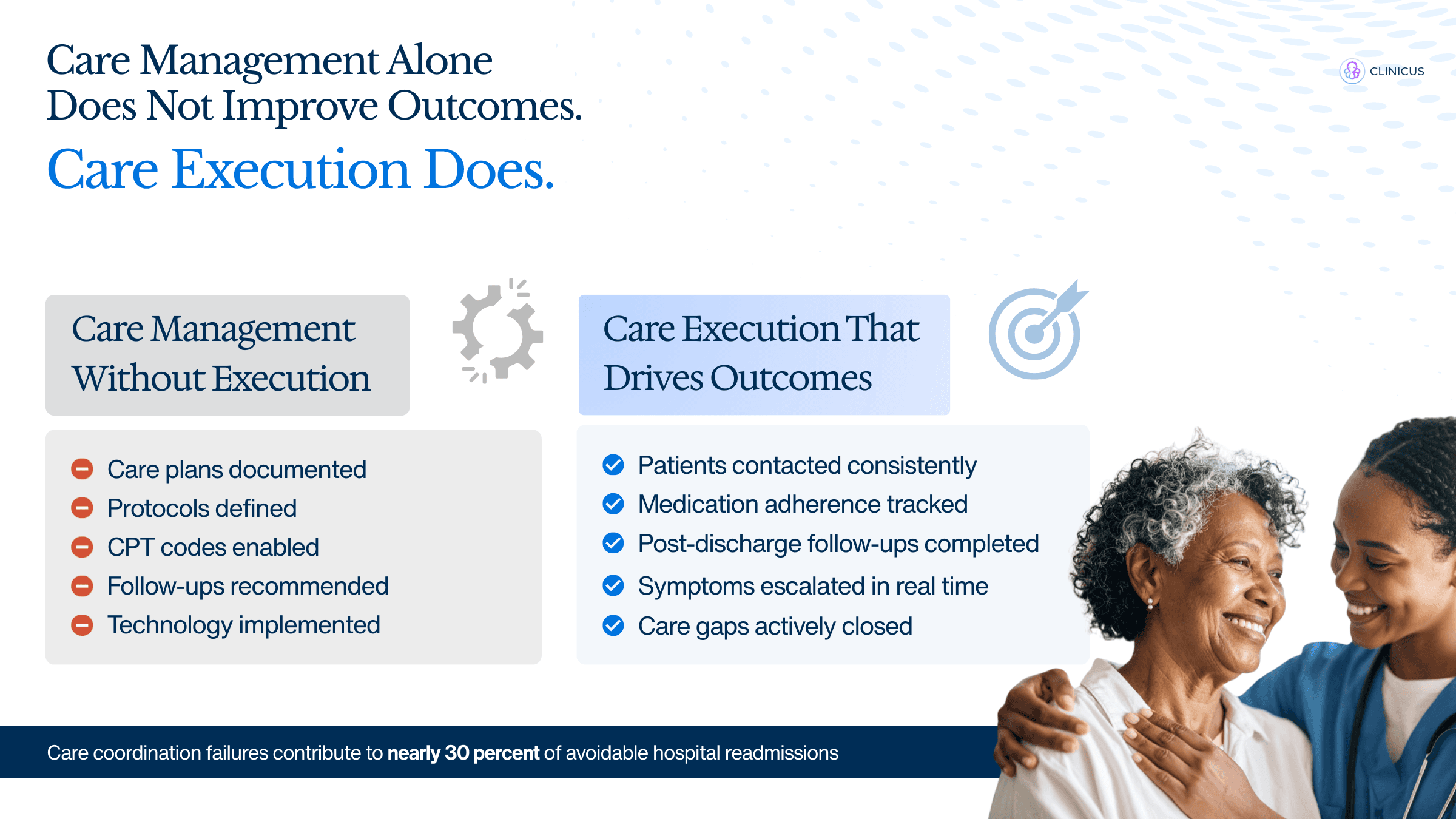
Care Management vs Care Execution
Care management focuses on planning, documentation, and tracking. This includes identifying high-risk patients, creating care plans, assigning tasks, and monitoring quality metrics.
Care execution is the operational layer. It is the day-to-day follow-through that turns plans into real clinical action. This includes timely outreach, responding to patient changes, escalating concerns, and coordinating providers around the patient.
Research shows that many care management programs struggle not because they lack staff or tools, but because execution breaks down between intention and action (AHRQ, Health Affairs).
Why Care Management Alone Falls Short
Multiple studies highlight that adding nurses or care coordinators without redesigning workflows does not consistently improve outcomes.
A review by the Agency for Healthcare Research and Quality (AHRQ) found that care management programs show mixed results when workflows, accountability, and escalation pathways are unclear.
The American Medical Association (AMA) has also noted that care teams often face alert fatigue, manual reviews, and disconnected systems, which slow response times and reduce effectiveness.
Common challenges include:
Patient alerts are reviewed too late to prevent escalation
Care tasks are spread across multiple systems and teams
Responsibility for follow-up is unclear
Nurses spend time tracking data instead of engaging patients
As a result, care teams become reactive rather than proactive.
What Care Execution Looks Like in Practice
Care execution bridges the gap between insight and action.
Effective execution ensures that when a patient’s condition changes, the care team knows quickly, understands what to do next, and acts without delay.
High-performing practices share several execution-focused traits:
Early visibility into patient changes using real-time data
Clear workflows that guide nurses on next steps
Defined escalation protocols for high-risk situations
Tight coordination between nurses, providers, and care teams
According to Health Affairs, programs that integrate care management with operational workflows show better outcomes, including fewer emergency visits and improved chronic condition control (Health Affairs).
Why Timeliness Matters More Than Volume
Many care management programs focus on the number of touchpoints or tasks completed. However, studies show that timing is more important than volume.
The Office of the National Coordinator for Health IT (ONC) emphasizes that delayed responses reduce the clinical value of patient data, even when information is accurate.
Care execution prioritizes speed and clarity:
Alerts that arrive early
Clear instructions on who acts and how
Immediate escalation when thresholds are crossed
This approach prevents small issues from becoming acute events.
Clinicus as an Operational Layer for Care Execution
Research consistently shows that care management programs succeed when insight is closely tied to action. Execution gaps often arise when patient data, clinical workflows, and accountability are disconnected.
Clincus is designed as an operational layer that focuses on how care is executed, not just how it is documented. Rather than adding another system for tracking or reporting, it structures the flow between patient signals, nurse activity, and provider response.
This design supports timely decision-making by ensuring that care teams see relevant changes early and understand the required next step. The emphasis is on reducing friction between identification of risk and clinical intervention.
How Clinicus Makes Patient Follow-Up Easy
Effective care execution depends on clarity. Nurses and care teams need to know which patients require attention, what action is expected, and when escalation is necessary.
Clincus supports this by aligning patient insights with defined workflows. Instead of relying on manual review or ad hoc follow-up, care activities are organized around priority and clinical relevance.
Key execution principles supported include:
Early visibility into patient risk and unmet care needs
Workflow-based guidance that reduces cognitive and administrative load
Defined escalation pathways for time-sensitive situations
Coordinated communication across nursing and provider teams
By structuring follow-through within daily operations, this approach enables care teams to act earlier and more consistently. The result is a shift from reactive intervention to proactive care delivery, which research associates with improved outcomes and lower utilization.
Conclusion
Care management is necessary, but it is not sufficient.
Practices that improve outcomes focus on building systems that support action. This means aligning technology, workflows, and human effort around execution.
When care teams have early insight, clear processes, and defined ownership, care becomes timely, coordinated, and reliable.
That is when care management delivers its true value.
Care management has become a standard part of modern healthcare. Most practices today have care coordinators, nurses, risk stratification tools, and documented care plans. Yet outcomes often remain unchanged. Hospitalizations continue, gaps in care persist, and staff feel stretched despite growing care management programs.
The difference is not effort or intent. It is execution.
Care management defines what should happen. Care execution ensures it actually happens, at the right time, for the right patient, by the right person.
Care Management vs Care Execution
Care management focuses on planning, documentation, and tracking. This includes identifying high-risk patients, creating care plans, assigning tasks, and monitoring quality metrics.
Care execution is the operational layer. It is the day-to-day follow-through that turns plans into real clinical action. This includes timely outreach, responding to patient changes, escalating concerns, and coordinating providers around the patient.
Research shows that many care management programs struggle not because they lack staff or tools, but because execution breaks down between intention and action (AHRQ, Health Affairs).
Why Care Management Alone Falls Short
Multiple studies highlight that adding nurses or care coordinators without redesigning workflows does not consistently improve outcomes.
A review by the Agency for Healthcare Research and Quality (AHRQ) found that care management programs show mixed results when workflows, accountability, and escalation pathways are unclear.
The American Medical Association (AMA) has also noted that care teams often face alert fatigue, manual reviews, and disconnected systems, which slow response times and reduce effectiveness.
Common challenges include:
Patient alerts are reviewed too late to prevent escalation
Care tasks are spread across multiple systems and teams
Responsibility for follow-up is unclear
Nurses spend time tracking data instead of engaging patients
As a result, care teams become reactive rather than proactive.
What Care Execution Looks Like in Practice
Care execution bridges the gap between insight and action.
Effective execution ensures that when a patient’s condition changes, the care team knows quickly, understands what to do next, and acts without delay.
High-performing practices share several execution-focused traits:
Early visibility into patient changes using real-time data
Clear workflows that guide nurses on next steps
Defined escalation protocols for high-risk situations
Tight coordination between nurses, providers, and care teams
According to Health Affairs, programs that integrate care management with operational workflows show better outcomes, including fewer emergency visits and improved chronic condition control (Health Affairs).
Why Timeliness Matters More Than Volume
Many care management programs focus on the number of touchpoints or tasks completed. However, studies show that timing is more important than volume.
The Office of the National Coordinator for Health IT (ONC) emphasizes that delayed responses reduce the clinical value of patient data, even when information is accurate.
Care execution prioritizes speed and clarity:
Alerts that arrive early
Clear instructions on who acts and how
Immediate escalation when thresholds are crossed
This approach prevents small issues from becoming acute events.
Clinicus as an Operational Layer for Care Execution
Research consistently shows that care management programs succeed when insight is closely tied to action. Execution gaps often arise when patient data, clinical workflows, and accountability are disconnected.
Clincus is designed as an operational layer that focuses on how care is executed, not just how it is documented. Rather than adding another system for tracking or reporting, it structures the flow between patient signals, nurse activity, and provider response.
This design supports timely decision-making by ensuring that care teams see relevant changes early and understand the required next step. The emphasis is on reducing friction between identification of risk and clinical intervention.
How Clinicus Makes Patient Follow-Up Easy
Effective care execution depends on clarity. Nurses and care teams need to know which patients require attention, what action is expected, and when escalation is necessary.
Clincus supports this by aligning patient insights with defined workflows. Instead of relying on manual review or ad hoc follow-up, care activities are organized around priority and clinical relevance.
Key execution principles supported include:
Early visibility into patient risk and unmet care needs
Workflow-based guidance that reduces cognitive and administrative load
Defined escalation pathways for time-sensitive situations
Coordinated communication across nursing and provider teams
By structuring follow-through within daily operations, this approach enables care teams to act earlier and more consistently. The result is a shift from reactive intervention to proactive care delivery, which research associates with improved outcomes and lower utilization.
Conclusion
Care management is necessary, but it is not sufficient.
Practices that improve outcomes focus on building systems that support action. This means aligning technology, workflows, and human effort around execution.
When care teams have early insight, clear processes, and defined ownership, care becomes timely, coordinated, and reliable.
That is when care management delivers its true value.
Browse Our Resources
Browse Our Resources
Browse Our Resources
Ready To Elevate Patient Care?
VBC@sciometrix.com
+1 833-799-8881
306 S Washington Ave, 6th Floor Royal Oak, Michigan - 48067
CARE MANAGEMENT
VALUE-BASED CARE
HEALTHCARE SOLUTIONS
Ready To Elevate
Patient Care?
VBC@sciometrix.com
+1 833-799-8881
306 S Washington Ave, 6th Floor Royal Oak, Michigan - 48067
CARE MANAGEMENT
VALUE-BASED CARE
HEALTHCARE SOLUTIONS
Ready To Elevate
Patient Care?
VBC@sciometrix.com
+1 833-799-8881
306 S Washington Ave, 6th Floor Royal Oak, Michigan - 48067
CARE MANAGEMENT
VALUE-BASED CARE
HEALTHCARE SOLUTIONS
Ready To Elevate Patient Care?
VBC@sciometrix.com
+1 833-799-8881
306 S Washington Ave, 6th Floor Royal Oak, Michigan - 48067
CARE MANAGEMENT
VALUE-BASED CARE
HEALTHCARE SOLUTIONS